Erectile dysfunction (ED) has evolved from a taboo subject whispered behind closed doors to a mainstream medical concern openly discussed in both clinics and commercials. Defined as the inability to achieve or maintain an erection sufficient for satisfactory sexual performance, ED is now recognized not only as a quality-of-life issue but also as a marker of systemic health. The rise of oral therapies such as sildenafil has revolutionized its treatment, making ED one of the most visible success stories in modern pharmacology. Yet the story is complex: understanding ED requires unpacking its physiology, risk factors, diagnostic approaches, and therapeutic strategies.
This article examines the scientific and clinical dimensions of ED with a focus on the pivotal role of phosphodiesterase type 5 (PDE5) inhibitors, alongside alternative and second-line treatments. Drawing on both foundational studies and clinical experience, we trace how ED moved from the margins of medical practice into the heart of men’s health.
The Scale of the Problem: Epidemiology and Public Health Relevance
Epidemiological data paint a striking picture of ED prevalence. The Massachusetts Male Aging Study, a landmark investigation of men aged 40–70, reported that more than half experienced some degree of erectile difficulty, with nearly 10% describing complete ED. Follow-up studies confirmed similar rates across populations, with Canadian surveys reporting comparable prevalence among men aged 18–70.
Several trends suggest that ED cases will continue to rise:
- An aging population
- Rising rates of diabetes and cardiovascular disease
- Increased longevity and higher quality-of-life expectations among aging men
Today, estimates suggest that millions of men worldwide live with recurrent erectile problems. Far from being an isolated condition, ED is increasingly recognized as a sentinel symptom of vascular health, predictive of coronary artery disease, hypertension, and metabolic syndrome. This link reframes ED as more than a sexual issue: it is a systemic health concern.
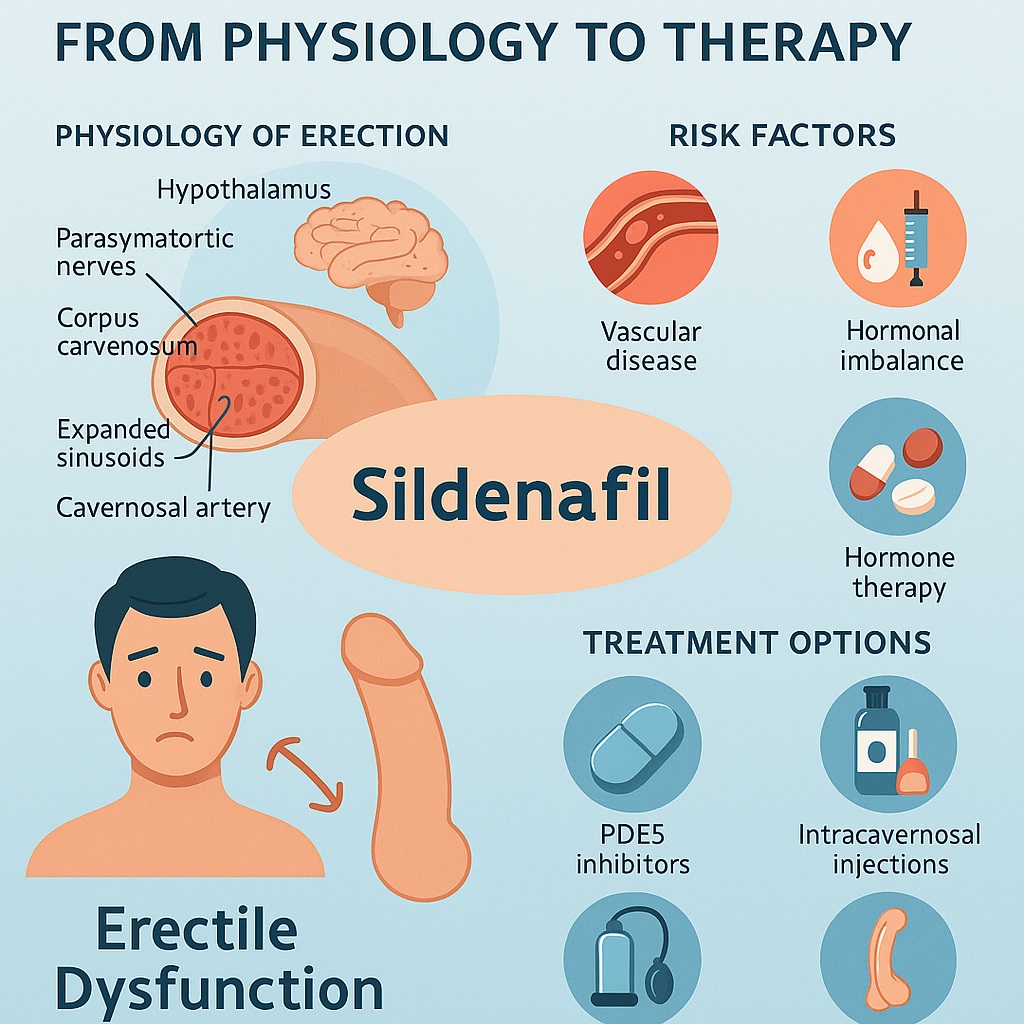
Physiology of Erection: A Delicate Balance
Erection is a marvel of integration between neural, vascular, and hormonal systems. In essence, it occurs when arterial inflow exceeds venous outflow, trapping blood within the corpora cavernosa.
Key mechanisms include:
- Neural control: Parasympathetic signals from sacral spinal nerves release nitric oxide (NO), initiating vasodilation; sympathetic input regulates detumescence.
- Vascular changes: Relaxation of cavernosal smooth muscle allows arterial blood to flood the sinusoids, which expand and compress venous outflow channels.
- Biochemical cascade: NO stimulates guanylate cyclase, increasing cyclic guanosine monophosphate (cGMP). Elevated cGMP lowers intracellular calcium, producing smooth muscle relaxation and penile rigidity.
Phosphodiesterase type 5 (PDE5) regulates this pathway by breaking down cGMP. The discovery that inhibiting PDE5 enhances erection laid the foundation for sildenafil and its successors. The clinical irony is irresistible: a molecule first tested for angina became the world’s most famous pill for intimacy.
Pathophysiology: Why Erections Fail
ED can arise from disruptions at any level of this integrated system. Once thought to be largely psychogenic, ED is now understood to be primarily organic in origin, especially among older men.
Common causes include:
- Vascular disease: Atherosclerosis accounts for nearly 40% of ED in men over 50. Risk factors mirror those of cardiovascular disease.
- Neurological disorders: Spinal cord injuries, neuropathies, and iatrogenic damage (e.g., post-prostatectomy) interfere with nerve conduction.
- Hormonal imbalance: Hypogonadism, thyroid disorders, or hyperprolactinemia reduce libido and modulate erectile function.
- Medications: Antihypertensives, antidepressants, and anti-androgens frequently impair sexual response.
- Systemic illness: Diabetes, renal failure, and chronic obstructive pulmonary disease contribute through multifactorial mechanisms.
Psychological and relational factors still matter, of course. Stress, depression, and performance anxiety can initiate or exacerbate ED, often overlapping with organic contributors.
Diagnosis: From Exhaustive to Streamlined
A generation ago, diagnosing ED required exhaustive biochemical panels, psychological testing, and invasive vascular assessments. With the advent of effective oral therapy, guidelines shifted toward a more minimalist, goal-oriented approach.
Core elements now include:
- A thorough medical and sexual history distinguishing ED from other dysfunctions such as premature ejaculation or loss of libido.
- Use of validated questionnaires, such as the International Index of Erectile Function (IIEF) or its abridged version, the SHIM, to quantify severity.
- Targeted physical examination focusing on vascular, neurological, and endocrine systems.
- Basic laboratory screening for diabetes, dyslipidemia, and—when indicated—testosterone and thyroid abnormalities.
Specialized investigations such as penile Doppler ultrasonography or selective arteriography are now reserved for select cases, such as young men with isolated vascular trauma who might be surgical candidates.
The Sildenafil Revolution: PDE5 Inhibitors as First-Line Therapy
The introduction of sildenafil in the late 1990s transformed ED management. By blocking PDE5, sildenafil prolongs cGMP activity, sustaining smooth muscle relaxation and blood flow during sexual stimulation. Clinical trials demonstrated dramatic efficacy: more than 80% of men reported improved erectile performance compared with less than half on placebo.
Sildenafil’s success ushered in an era where oral pharmacotherapy became first-line treatment, displacing invasive injections and cumbersome vacuum devices. Over time, other PDE5 inhibitors expanded the therapeutic arsenal:
- Vardenafil: Demonstrated effectiveness in post-prostatectomy patients and men with diabetes, traditionally difficult-to-treat groups.
- Tadalafil: Distinguished by its 17.5-hour half-life, allowing flexibility and “weekend coverage.” It is less affected by food or alcohol intake, making it practical for daily or situational use.
Together, these agents offered men not only functional erections but also restored confidence, intimacy, and quality of life.
Safety, Contraindications, and Cautions
Concerns about cardiovascular safety accompanied the introduction of PDE5 inhibitors. However, large reviews found no significant increase in myocardial infarction or sudden death among users compared with placebo.
Important considerations include:
- Contraindication with nitrates: The combination can cause profound hypotension.
- Caution in polypharmacy: Drugs affecting cytochrome P450 3A4, such as erythromycin or ketoconazole, can raise PDE5 inhibitor levels.
- Elderly and comorbid patients: Dose adjustments may be required in renal or hepatic impairment.
Side effects are generally mild—headache, flushing, dyspepsia, and nasal congestion predominate. Priapism remains rare, and fears about fertility effects have not been substantiated in long-term studies.
Beyond Pills: Second-Line and Alternative Therapies
While PDE5 inhibitors dominate, they are not universal cures. Nonresponders or contraindicated patients may benefit from alternative options:
- Alprostadil (prostaglandin E1): Administered intraurethrally or via intracavernosal injection, it directly induces cavernosal smooth muscle relaxation. Pain and invasiveness limit acceptance.
- Combination injections: Mixtures of papaverine, phentolamine, and alprostadil increase efficacy while lowering individual drug doses.
- Vacuum erection devices: Non-invasive, though satisfaction rates vary due to mechanical inconvenience.
- Surgical implants: Reserved for refractory cases, penile prostheses provide reliable erections but are invasive and irreversible.
These therapies, though less celebrated than sildenafil, remain vital in comprehensive ED management.
ED as a Window Into Men’s Health
Perhaps the most profound lesson of ED research is its role as a sentinel marker of systemic disease. Vascular ED often precedes clinical cardiovascular disease by several years, offering clinicians an early warning signal. Screening for diabetes, hypertension, and lipid disorders in men presenting with ED is now considered best practice. In this sense, sildenafil prescriptions may double as cardiovascular risk assessments—a clever form of opportunistic medicine.
Conclusion: From Taboo to Therapeutic Triumph
The story of erectile dysfunction is a triumph of medical progress and a case study in reframing disease. Once stigmatized and hidden, ED is now understood as a common, treatable, and medically significant condition. The advent of PDE5 inhibitors—spearheaded by sildenafil—transformed both treatment and societal attitudes.
Yet the journey is ongoing. For some men, oral therapy is insufficient; for others, ED heralds deeper vascular or endocrine pathology requiring systemic management. The future lies in more personalized, integrative care that views ED not as an isolated defect but as part of broader men’s health.
FAQ
1. How effective is sildenafil for erectile dysfunction?
Sildenafil improves erections in 60–80% of men, with success rates varying by comorbidities such as diabetes or prostate surgery.
2. Are PDE5 inhibitors safe for men with heart disease?
Yes, in most cases. However, they are contraindicated with nitrates and should be used cautiously in severe cardiovascular disease under medical supervision.
3. What happens if PDE5 inhibitors do not work?
Alternative therapies include alprostadil, intracavernosal injections, vacuum devices, or penile implants. Addressing underlying conditions like diabetes or low testosterone can also restore responsiveness.
4. Is erectile dysfunction always a psychological issue?
No. While psychological factors play a role, most ED in older men has an organic basis—vascular, neurological, or hormonal. It is often a sign of systemic disease.